As occupational therapists, we know that home modifications can be transformative for our clients. But what does the latest research tell us about where we’re succeeding—and where we need to grow? A comprehensive systematic review published in March 2025 examined 20 studies on home modifications for aging in place, revealing both encouraging evidence and critical gaps that should shape how we approach this work (Cha, 2025).
What the Research Confirms
The good news? The evidence supporting home modifications is strong. Among the 20 studies analyzed, 13 (65%) confirmed the effectiveness of home modifications in three key areas: fall prevention, functional independence, and cost savings (Cha, 2025). This aligns with what many of us see in practice—thoughtful environmental modifications can dramatically improve our clients’ safety and quality of life.
The review found that home modifications extend beyond simple physical safety interventions (Cha, 2025). Studies documented improvements in functional performance, reduced nursing home admissions, enhanced quality of life, and decreased caregiver burden (Cha, 2025). These findings validate the holistic, person-environment-occupation approach that occupational therapy brings to home modification work.

The Critical Gaps: Where We Need to Lead
Here’s where it gets interesting for us as clinicians. The systematic review identified three significant gaps in current home modification research and practice (Cha, 2025):
Personalized Interventions
While occupational therapy prides itself on client-centered, individualized care, the research shows that few studies have examined personalized intervention approaches in home modifications (Cha, 2025). Most existing research focuses on standardized modifications—grab bars, ramps, improved lighting—without adequately exploring how modifications can be tailored to individual lifestyles, cultural preferences, health trajectories, and occupational goals (Cha, 2025).
This represents a significant opportunity for occupational therapists. Our training in activity analysis, occupational profiles, and the PEO (Person-Environment-Occupation) model positions us uniquely to develop and implement truly personalized home modification strategies (Cha, 2025). Rather than applying a one-size-fits-all checklist, we can assess how a client’s specific activities, routines, roles, and future needs should drive modification decisions.
Smart Home Technologies
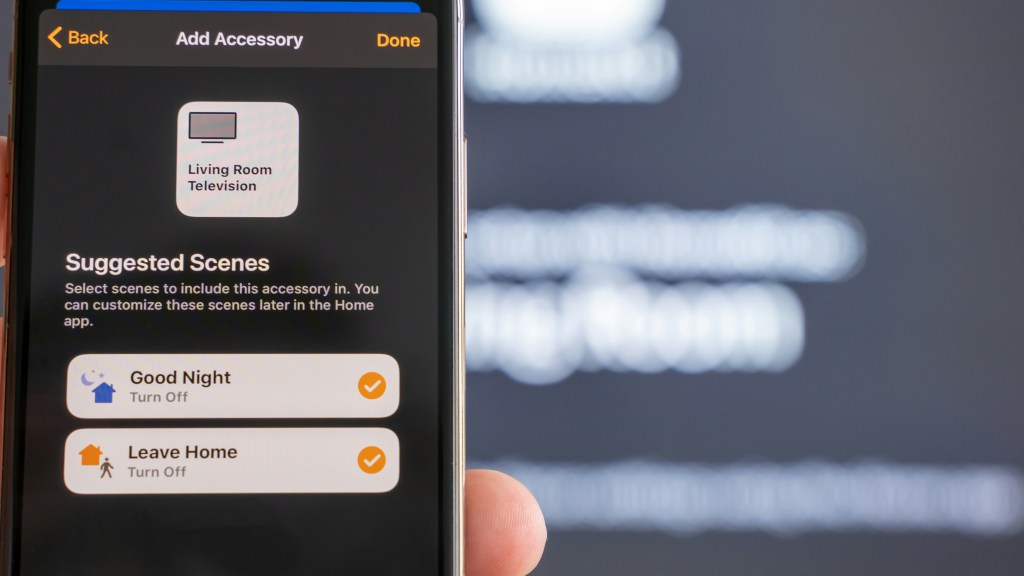
The integration of technology into home modification strategies remains under-explored in the literature (Cha, 2025). While traditional low-tech modifications like grab bars and threshold ramps continue to be valuable, emerging smart home technologies offer new possibilities for supporting aging in place (Cha, 2025).
Smart home innovations might include motion-sensor lighting systems, fall detection devices, voice-activated environmental controls, automated medication reminders, and remote monitoring systems that alert caregivers to potential safety concerns (Cha, 2025). However, research examining the effectiveness, usability, cost-effectiveness, and integration of these technologies with traditional modifications is limited (Cha, 2025).
As occupational therapists, we need to become fluent in both low-tech and high-tech solutions, understanding when and how to recommend technology that enhances rather than complicates our clients’ daily lives.
Long-Term Adaptability
Perhaps the most significant gap identified in the review is the lack of research on long-term adaptability of home modifications (Cha, 2025). Most studies evaluate short-term outcomes—typically 3 to 12 months post-modification—but few examine how modifications perform as clients’ functional abilities change over time (Cha, 2025).
This is particularly relevant for progressive conditions like Parkinson’s disease, dementia, or multiple sclerosis, where functional abilities may decline gradually. One longitudinal study in the review followed individuals with Parkinson’s disease over three years and found that while some modifications (like grab bars in hygiene areas) remained helpful, new barriers emerged over time, particularly in outdoor spaces (Andersson et al., 2023; Cha, 2025).
Occupational therapists need to shift from thinking about home modifications as one-time interventions to viewing them as dynamic, evolving strategies that anticipate future needs. This requires us to consider disease trajectories, plan for progressive changes, and build flexibility into modification recommendations.
Actionable Steps for Therapists
Based on these research findings, here are concrete ways you can enhance your home modification practice:
Deepen Your Personalization Approach
- Conduct comprehensive occupational profiles that explore clients’ valued activities, daily routines, cultural backgrounds, and long-term goals before recommending modifications
- Use standardized assessments like the Canadian Occupational Performance Measure (COPM) to identify client-prioritized concerns rather than relying solely on safety checklists
- Document how each recommended modification connects to specific occupational performance goals, not just general safety improvements
Expand Your Technology Knowledge
- Familiarize yourself with current smart home technologies available for aging in place, including their costs, installation requirements, and evidence base
- Partner with technology specialists, contractors, and vendors who can help implement integrated low-tech and high-tech solutions
- Stay current on emerging assistive technologies through continuing education and professional development
Plan for Progressive Changes
- When assessing clients with progressive conditions, research typical disease trajectories and anticipate future functional changes
- Recommend modifications that can be adapted or expanded over time rather than requiring complete renovation later
- Consider universal design principles that provide flexibility for changing needs
- Schedule follow-up assessments at appropriate intervals based on diagnosis and functional trajectory
Enhance Your Documentation
- Document not just what modifications were recommended, but why they were chosen based on the client’s specific occupational profile
- Include baseline and outcome measures that demonstrate effectiveness in multiple domains: falls, functional independence, quality of life, and caregiver burden
- Contribute to the evidence base by tracking long-term outcomes when possible
Collaborate Interdisciplinarily
- Build relationships with architects, contractors, interior designers, and technology specialists who understand aging-in-place principles
- Develop referral networks that include funding specialists who can help clients access financial resources for modifications
- Participate in community aging-in-place initiatives and policy discussions
Invest in Your Expertise
The gaps identified in this research highlight why specialized training in home modifications is essential for occupational therapists who want to provide truly comprehensive services. While our entry-level education provides foundational knowledge of environmental modifications, advanced practice in this area requires deeper expertise in assessment, technology integration, building codes, funding mechanisms, and business development.
The Certified Home Accessibility Therapist (CHAT) program offers AOTA-approved training specifically designed to address these knowledge gaps. Built exclusively for occupational therapists and occupational therapy assistants, CHAT provides evidence-based education on conducting thorough home assessments, integrating client goals and preferences, navigating funding and regulatory challenges, and launching or expanding a home modification practice. The program includes 30 contact hours of professional development, ongoing mentorship, case reviews, and a network of practicing therapists who can support your growth in this specialty area.
Learn more about the CHAT program and how it can help you bridge the gap between current research and advanced practice: https://www.thehomeaccessibilitytherapist.com/CHAT
Moving Forward
This systematic review reminds us that while we have solid evidence supporting home modifications for fall prevention and functional independence, we have significant opportunities to advance the field. As occupational therapists, we are ideally positioned to lead innovation in personalized interventions, technology integration, and long-term adaptable solutions.
By staying current with emerging research, investing in specialized training, and advocating for comprehensive, client-centered approaches, we can ensure that home modifications truly support our clients’ goals of aging in place safely, independently, and meaningfully.
References
Andersson, M., Lindgren, I., Hamnegård, H., & Malmgren Fänge, A. (2023). Environmental barriers and housing accessibility problems for people with Parkinson’s disease: A three-year perspective. Scandinavian Journal of Occupational Therapy, 30(3), 371-381. https://doi.org/10.1080/11038128.2022.2042022
Cha, S. M. (2025). A systematic review of home modifications for aging in place in older adults. Healthcare, 13(7), 752. https://doi.org/10.3390/healthcare13070752
Ready to take your home modification practice to the next level? Join our Facebook community for ongoing discussions on home accessibility and safety: https://www.facebook.com/groups/homeaccessibilitysafety
Leave a comment