I hear it all the time: “Sue, I’m burned out from traditional therapy. I just want to do home modification assessments—go in, evaluate, make recommendations, and move on to the next client.” I understand the appeal. After years of grinding through productivity standards, insurance denials, and documentation demands, the idea of conducting independent assessments sounds like freedom.
But here’s the truth: If you’re approaching home modifications as one-time transactions, you’re not really practicing occupational therapy. And you’re missing the opportunity to provide the kind of transformative, relationship-based care that makes this work both clinically meaningful and financially sustainable.
The Appeal of the Quick Assessment Model
Let’s be honest about why therapists are drawn to one-off home assessments. The traditional medical model has left many of us exhausted. We’re tired of:
- Meeting unrealistic productivity requirements that prioritize billing units over quality care
- Fighting with insurance companies for authorization of services we know clients need
- Spending more time on documentation than with clients
- Working within systems that don’t value our clinical reasoning or expertise
The promise of conducting independent home modification assessments—setting your own schedule, being your own boss, getting paid directly by clients—sounds like the antidote to all that burnout. And to some degree, it can be.
But if we simply replicate the transactional, checklist-driven approach we’re trying to escape, we haven’t really changed anything. We’ve just traded one limited practice model for another.
What the Research Reveals
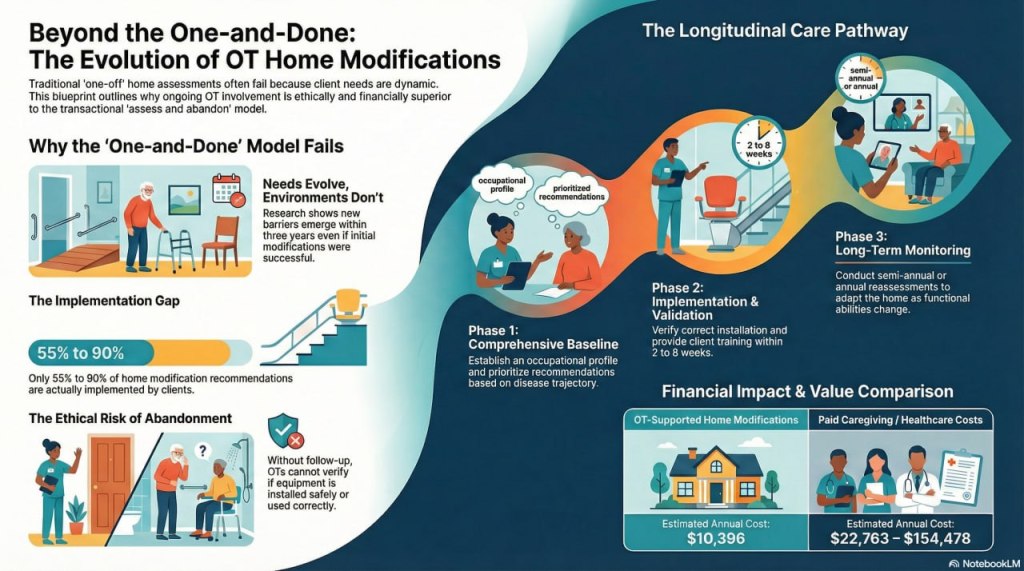
A 2025 systematic review of home modifications for aging in place examined 20 studies and found something striking: most research evaluates outcomes only 3 to 12 months post-modification (Cha, 2025). Few studies examine how modifications perform as clients’ functional abilities change over time, yet this is precisely when ongoing occupational therapy expertise becomes most valuable (Cha, 2025).
Consider the longitudinal research that does exist. Andersson et al. (2023) followed individuals with Parkinson’s disease over three years after home modifications were implemented. While some modifications—like grab bars in bathrooms—remained helpful throughout the study period, new environmental barriers emerged as the disease progressed, particularly in outdoor spaces and with more complex mobility tasks (Andersson et al., 2023).
The one-time assessment conducted at baseline couldn’t anticipate these evolving needs. Clients who received modifications based on their Year 1 functional status found themselves struggling with new barriers by Year 3—barriers that could have been anticipated and planned for by a therapist who understood Parkinson’s disease progression and maintained an ongoing relationship with the client (Andersson et al., 2023).
This isn’t unique to Parkinson’s disease. Research on place-based occupational therapy demonstrates that therapists achieve superior outcomes when they familiarize themselves with clients’ routines, habits, and everyday activities over time, allowing them to contextualize recommendations and adapt interventions as circumstances change (Taylor et al., 2025). Single-visit assessments simply cannot capture this depth of understanding.
The Clinical Reality: Needs Evolve
Think about the clients you’ve worked with who have progressive conditions—multiple sclerosis, dementia, chronic heart failure, rheumatoid arthritis, macular degeneration. Their functional abilities don’t remain static. What they need from their home environment at diagnosis looks very different from what they need two, five, or ten years later.
A comprehensive home modification assessment conducted today might recommend:
- A walk-in shower with grab bars and a shower bench
- Improved lighting in hallways and stairways
- Removal of throw rugs and tripping hazards
- Lever-style door handles instead of knobs
These are valuable modifications. But what happens 18 months later when:
- The client’s balance has deteriorated and they now need a rolling walker that won’t fit through the bathroom doorway you measured when they were using a cane?
- Their cognitive changes mean they’re getting confused about operating the new shower controls you recommended?
- Their vision has declined to the point where the lighting improvements are no longer sufficient?
- They’re having difficulty with the stairs you determined were “manageable with a railing”?
If you conducted a one-time assessment and moved on, who is addressing these evolving needs? Often, no one—until a fall or crisis forces the family to make emergency decisions without the benefit of professional guidance.
The Ethical Implications of “Assess and Abandon”
Here’s what makes me uncomfortable about the one-and-done model: it’s not really client-centered care. It’s task-centered care. We’re completing an assessment task, delivering recommendations, and considering our job done—regardless of whether those recommendations continue to meet the client’s occupational needs over time.
Research on adherence to home modification recommendations shows significant variation, with implementation rates ranging from 55% to 90% (Harper et al., 2021). Many factors influence whether clients actually implement recommendations, including cost, family support, emotional readiness, and understanding of the rationale behind modifications (Harper et al., 2021).
If we deliver recommendations and disappear, we have no idea whether:
- Clients understood and agreed with our suggestions
- They had the financial resources to implement them
- The modifications were actually installed correctly
- The modifications are being used as intended
- The modifications continue to meet their needs as abilities change
We’re essentially practicing occupational therapy without measuring outcomes—something we’d never accept in any other practice setting.
Our Professional Obligation to Verify Outcomes
Beyond the long-term need for reassessment as conditions change, there’s a more immediate ethical obligation that one-time assessments fail to address: we have a professional responsibility to ensure that our recommendations actually work and that clients know how to use them safely and effectively.
The Occupational Therapy Code of Ethics obligates us to “ensure that the outcomes of our interventions are beneficial to recipients” (American Occupational Therapy Association, 2020). Yet if we complete an assessment, hand over recommendations, and never return, how can we possibly fulfill this obligation?
Consider what can go wrong between recommendation and implementation:
Installation Issues
- Grab bars installed in incorrect locations or at wrong heights
- Ramps built at unsafe slopes or without proper railings
- Equipment installed that doesn’t match the specifications you recommended
- Modifications that technically meet your written recommendation but don’t actually support the functional activity you intended
Equipment Misuse
- Clients who don’t understand how to properly use a transfer bench or shower chair
- Caregivers who aren’t trained on safe transfer techniques using new grab bars
- Confusion about when and how to use adaptive equipment
- Safety features that aren’t being utilized because no one explained their purpose
Unintended Consequences
- Modifications that solve one problem but create another (e.g., a raised toilet seat that makes it harder to stand up)
- Equipment that interferes with other daily activities you didn’t anticipate
- Changes that family members or caregivers find difficult to navigate
- Modifications that the client simply won’t use because they don’t fit their routines or preferences
A study on adherence to home modification recommendations found that even when clients invest in implementing changes, adherence rates vary significantly—and one key barrier is inadequate training and follow-up from the recommending therapist (Harper et al., 2021). Clients may complete modifications but not use them correctly, or they may abandon them entirely because they don’t understand the rationale or proper technique (Harper et al., 2021).
We would never accept this in any other occupational therapy setting. Imagine recommending a splint for a client and never following up to see if it fits properly, if they’re wearing it correctly, or if it’s actually improving function. We’d consider that incomplete care—potentially even negligent. Yet some therapists think it’s acceptable practice in home modifications.
At minimum, ethical practice requires:
- Implementation verification: Confirming that recommended modifications were installed correctly and meet safety standards
- Client and caregiver training: Teaching proper use of new equipment, environmental features, and safety strategies
- Functional validation: Observing the client actually performing relevant activities using the modifications to ensure they work as intended
- Problem-solving: Addressing any issues, barriers, or unintended consequences that emerge during real-world use
- Outcome measurement: Documenting whether the modifications achieved the intended goals for occupational performance and safety
This isn’t “extra” service—it’s fundamental clinical practice. If we’re not following up to ensure our recommendations are implemented correctly and are actually helping, we’re not really practicing occupational therapy. We’re just generating paperwork.
The ethical responsibility to verify outcomes isn’t just about long-term disease progression—it starts the moment we make a recommendation. One-time assessments without follow-up fail this basic professional obligation.
What Longitudinal Home Modification Practice Looks Like
Shifting from transactional assessments to ongoing therapeutic relationships doesn’t mean you’re trapped back in the productivity-driven medical model. It means structuring your practice to support clients across time in a way that’s both clinically sound and financially sustainable.
Here’s what this might look like in practice:
Initial Comprehensive Assessment
- Thorough occupational profile exploring valued activities, daily routines, cultural preferences, and long-term goals
- Detailed environmental assessment using standardized tools
- Diagnosis-specific understanding of likely disease trajectory and functional changes
- Recommendations prioritized by urgency, impact, and client readiness
- Clear documentation of baseline functional abilities and occupational performance
Implementation Support (Week 2-8)
- Consultation with contractors, family members, or other professionals implementing modifications
- Review of plans and specifications to ensure they match clinical recommendations
- Problem-solving when recommended modifications aren’t feasible due to structural, financial, or other constraints
- Training clients and caregivers on proper use of new equipment or environmental features
Short-Term Follow-Up (3-6 Months)
- Assessment of which recommendations were implemented and which weren’t
- Evaluation of whether modifications are being used correctly and effectively
- Measurement of outcomes: functional performance, falls, quality of life, caregiver burden
- Adjustment or addition of recommendations based on actual lived experience
- Documentation of progress and ongoing needs
Long-Term Monitoring (Annually or Semi-Annually)
- Reassessment of functional abilities and occupational performance
- Evaluation of whether existing modifications continue to meet needs
- Anticipatory planning for expected changes based on disease progression or aging
- Recommendations for additional or modified interventions
- Connection to community resources, funding sources, or other supports
This model allows you to maintain the autonomy, flexibility, and independence you’re seeking while providing the kind of comprehensive, outcomes-driven care that actually changes lives.
The Business Case for Ongoing Relationships
I know what some of you are thinking: “But Sue, I can’t make a living doing follow-up visits with the same clients. I need new referrals to stay financially viable.”
Let me challenge that assumption. Consider the business costs of constantly seeking new clients:
- Marketing expenses to attract new referrals
- Time spent on intake, scheduling, and administrative processes for each new client
- Lack of efficiency that comes from working with unfamiliar clients, homes, and family systems
- No opportunity for word-of-mouth referrals from satisfied clients you’ve abandoned after one visit
Now consider the benefits of longitudinal relationships:
- Increased efficiency because you already know the client, their home, and their needs
- Higher client satisfaction because you’re providing genuine relationship-based care
- Strong word-of-mouth referrals from clients and families who trust you and value ongoing support
- Opportunity to bill for services that have clear clinical justification (reassessments, equipment trials, caregiver training)
- Ability to anticipate needs and recommend modifications gradually as budget allows rather than overwhelming clients with extensive one-time costs
A 2025 study examining home modification outcomes found that interventions supported by occupational therapists resulted in mean modification costs of $10,396.65, substantially less than annual healthcare or paid caregiving costs ranging from $22,763 to $154,478 (Chan & Pynoos, 2025). When therapists maintain relationships with clients over time, they can stage modifications strategically, helping clients invest in the most impactful changes first and adding additional modifications as needs evolve and resources allow (Chan & Pynoos, 2025).
This approach is actually more financially accessible for clients and creates ongoing revenue streams for your practice.
Reframing Your Value Proposition
When therapists tell me they want to “just do assessments,” I often hear an underlying belief that assessment is the valuable part of what we do, and everything else is tedious follow-through. But that’s backward.
Assessment is important, but it’s only the beginning. Our real value as occupational therapists lies in:
- Understanding the relationship between person, environment, and occupation over time
- Anticipating how functional changes will impact occupational performance
- Problem-solving when initial recommendations don’t work as expected
- Adapting interventions based on real-world implementation and outcomes
- Educating clients and caregivers so they can make informed decisions about their environment
- Advocating for modifications that support meaningful activities, not just safety checklists
This expertise isn’t delivered in a single assessment. It unfolds across a therapeutic relationship.
Research confirms that occupational therapists working in home environments achieve superior functional outcomes compared to clinic-based services, and significantly reduce hospital readmissions, emergency department visits, and nursing home placements (Leland et al., 2025). But these outcomes weren’t achieved through one-time visits—they resulted from occupational therapists who stayed engaged with clients, monitored changes, and adapted interventions over time (Leland et al., 2025).
Practical Steps to Shift Your Practice Model
If you’re currently offering one-time assessments or considering moving into home modification work, here’s how to structure your practice for ongoing client relationships:
Set Clear Service Packages
- Offer tiered service options that include initial assessment plus defined follow-up points (e.g., “Comprehensive Package: Initial assessment + 3-month follow-up + annual reassessment”)
- Price packages to reflect the value of longitudinal care while remaining competitive
- Clearly communicate to clients why follow-up is clinically necessary, not just an upsell
Develop Diagnosis-Specific Protocols
- Create anticipated timelines for follow-up based on common diagnoses (e.g., Parkinson’s disease might warrant semi-annual reassessments; stable arthritis might need annual check-ins)
- Use evidence-based understanding of disease progression to explain why ongoing monitoring is important
- Document protocols so clients understand this is standard clinical practice, not arbitrary
Use Outcome Measures Consistently
- Administer standardized assessments at baseline and follow-up visits to demonstrate change over time
- Track falls, functional performance, quality of life, and other relevant outcomes
- Share outcome data with clients and referral sources to demonstrate the value of ongoing therapy involvement
Build Follow-Up Into Your Workflow
- Schedule follow-up appointments before clients leave the initial assessment
- Use automated reminders (email, text, phone) to stay connected with clients between visits
- Create simple check-in protocols (brief phone calls or questionnaires) to monitor status between formal reassessments
Educate Clients and Referral Sources
- Include information about the importance of longitudinal home modification services in your marketing materials
- Share research showing that one-time assessments miss evolving needs
- Position yourself as a long-term partner in supporting aging in place, not a one-time consultant
Network With Progressive Care Providers
- Build relationships with neurologists, geriatricians, and other physicians who understand progressive conditions
- Partner with care managers, elder law attorneys, and aging life care professionals who coordinate long-term support
- Join aging-in-place coalitions and organizations that value comprehensive, ongoing services
Moving From Transactions to Transformation
Occupational therapy at its best is about supporting clients’ engagement in meaningful activities across their lifespan. Home modifications aren’t isolated interventions—they’re tools that enable occupation. And occupation changes as people change.
If we reduce our role to conducting one-time assessments, we’re functioning more like home inspectors than occupational therapists. We’re forfeiting the clinical reasoning, relationship-building, and adaptive problem-solving that make our profession unique and valuable.
The therapists I see building the most successful, sustainable, and satisfying home modification practices aren’t the ones doing quick assessments and moving on. They’re the ones who develop genuine relationships with clients and families, who stay involved as needs evolve, who celebrate when modifications enable clients to continue living independently, and who problem-solve when challenges arise.
This is the work that will sustain you professionally—not just financially, but emotionally and clinically. This is what occupational therapy looks like when we practice it with the depth, expertise, and client-centeredness our profession was founded on.
Invest in Expertise That Supports This Model
Shifting from transactional assessments to longitudinal home modification practice requires both mindset change and skill development. You need to understand disease trajectories, anticipatory planning, business structures that support ongoing relationships, and communication strategies that help clients understand the value of continued involvement.
The Certified Home Accessibility Therapist (CHAT) program provides comprehensive training in these areas, including modules on assessment across the lifespan, working with progressive conditions, ethical decision-making, business development, and building sustainable practice models. With 30 contact hours of AOTA-approved education, ongoing mentorship, and a community of practitioners committed to excellence in home modification practice, CHAT helps you develop the expertise to provide truly transformative care.
Learn more: https://www.thehomeaccessibilitytherapist.com/CHAT
The Bottom Line
Occupational therapists need to shift from thinking about home modifications as one-time interventions to viewing them as dynamic, evolving strategies that anticipate future needs. This isn’t just better for clients—it’s better for your practice, your professional satisfaction, and the long-term viability of home modification services.
The one-and-done model might feel like an escape from burnout, but it’s a hollow substitute for the meaningful, relationship-based practice most of us entered this profession to provide. Let’s build something better—for our clients and for ourselves.
References
Andersson, M., Lindgren, I., Hamnegård, H., & Malmgren Fänge, A. (2023). Environmental barriers and housing accessibility problems for people with Parkinson’s disease: A three-year perspective. Scandinavian Journal of Occupational Therapy, 30(3), 371-381. https://doi.org/10.1080/11038128.2022.2042022
Cha, S. M. (2025). A systematic review of home modifications for aging in place in older adults. Healthcare, 13(7), 752. https://doi.org/10.3390/healthcare13070752
Chan, A. W., & Pynoos, J. (2025). Home modification outcomes for adults aged 50 years and over: A scoping review. OTJR: Occupation, Participation and Health, 45(3), 456-468. https://doi.org/10.1177/15394492251361086
Harper, K. J., Barton, C., & Haines, T. (2021). Improving adherence to home modification recommendations: A systematic review. Disability and Rehabilitation, 43(16), 2289-2298. https://doi.org/10.1080/09638288.2019.1700293
Leland, N. E., Elliott, S. J., O’Malley, L., & Murphy, S. L. (2025). The value of occupational therapy in the home environment: Educating families and caregivers. American Journal of Occupational Therapy, 79(2), 7902180020. https://doi.org/10.5014/ajot.2025.050231
Taylor, R. R., Lee, S. W., & Braveman, B. (2025). The potential of place-based occupational therapy to support aging in place: A scoping review. BMC Public Health, 25, 1847. https://doi.org/10.1186/s12889-025-21038-3
Ready to transform your home modification practice? Join our Facebook community for ongoing discussions: https://www.facebook.com/groups/homeaccessibilitysafety
Leave a comment